Illnesses and deaths from food outbreaks skyrocketed in 2024, report finds
Hospitalizations and deaths from foodborne illnesses more than doubled in 2024 over the prior year, with most people sickened in a small number of high-profile outbreaks involving lunch meat, eggs, cucumbers and other commonly consumed foods, according to a report published Thursday.
The report comes as some US lawmakers are pushing legislation that would bar the US Department of Agriculture (USDA) from implementing a new regulatory framework proposed under former President Joe Biden aimed at addressing Salmonella contamination in raw poultry.
A total of 1,392 were sickened from contaminated food in 2024, up from 1,1118 people in 2023, and the health impacts of the outbreaks was more severe, with 487 people hospitalized last year compared to 230 the previous year. Nineteen people died after eating contaminated food in 2024, compared to eight in 2023, according to the report.
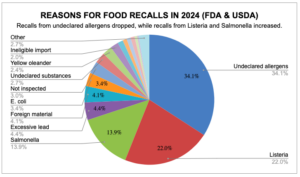
Across 13 total outbreaks in 2024, almost all of the illnesses were caused by E. coli, Listeria, and Salmonella bacteria, including a large outbreak of illnesses tied to E. coli contaminated onions in McDonald’s Quarter Pounder burgers. A large outbreak that landed 60 people in the hospital was linked to listeria-contaminated products traced back to a now-shuttered Boar’s Head plant in Virginia. The number of food recalls because of Listeria, Salmonella or E. coli increased significantly in 2024, representing 39% of all recalls.
“This report serves as an important reminder that there cannot be any cuts to food safety funding or rollbacks in regulations,” said Brian Ronholm, the director of food policy for the nonprofit Consumer Reports who was not involved in the study. “Industry, regulators and consumers must be constantly vigilant about food safety and the data in this report shows that there is still much work to be done and improvements to be made.”
One of 2024’s worst outbreaks came from an unexpected source – edible mushroom products used for “microdosing,” a trend that involves consuming tiny quantities of the psychedelic drugs to enhance mood and creativity. The US Food and Drug Administration (FDA) linked 180 illnesses to chocolate snacks containing mushrooms, with 73 people hospitalized and 3 deaths, according to the report.
“That’s not something that’s necessarily top of mind for most folks thinking about food safety,” said Stanton Cope, a Consumer Watchdog associate with the US PIRG Education Fund and an author of the report. “We just want to make sure people are considering everything that’s going into their bodies.”
A combination of factors may be to blame for the elevated number of illnesses in 2024, Cope said, including potentially higher concentrations of bacteria in contaminated foods and a time lag between the first illnesses of an outbreak and associated food recalls issued to alert stores and consumers.
 Food recalls, actions to remove foods from the market that violate the FDA’s regulations, can occur when products are found to contain harmful bacteria, viruses or parasites or foreign objects such as metal or plastic, or when companies fail to add allergens such as peanuts to labels. Most of the time, the food manufacturer or distributor voluntarily initiate recalls, although the FDA sometimes mandates them.
Food recalls, actions to remove foods from the market that violate the FDA’s regulations, can occur when products are found to contain harmful bacteria, viruses or parasites or foreign objects such as metal or plastic, or when companies fail to add allergens such as peanuts to labels. Most of the time, the food manufacturer or distributor voluntarily initiate recalls, although the FDA sometimes mandates them.
Despite the severity of foodborne illness outbreaks last year and the increase in recalls tied to Salmonella, E. coli and Listeria, the overall number of food recalls in 2024 dropped about 5% to 296 last year.
Recalls for undeclared allergens in foods accounted for more than a third of all recalls last year, though they dropped to 101 in 2024 from 154 in 2023.
“We find that encouraging,” said Teresa Murray, consumer watchdog director at the US PIRG Education Fund and an author of the report. “Maybe food manufacturers are getting better at declaring allergens. There’s only nine to keep track of, it’s not that difficult. That seems like it should be one of the easiest issues for food manufacturers to deal with.”
Neither the FDA nor USDA require companies to contact grocery stores or restaurants to inform them when a product has been recalled, although groceries often learn about recalls from their suppliers before public notices are posted by the federal agencies, according to the report. Companies are not required to notify consumers about recalls.
“We recounted many cases from last year where it was weeks and sometimes months after a recall and people were still getting sick,” said Murray. “I don’t think that they knew.”
“In some cases, we would like to see the FDA and the [US Department of Agriculture] to do a little bit more to pressure all of the stakeholders to do a better job of communicating to the public,” she added. “We would like to see stores become more active and consumers pay more attention.”
(Featured image by Julia Bogdonova via Unsplash+.)
 EWG
EWG


